ATS 2024

-
Mycobacterium Abscessus and Klebsiella Oxytoca Co-Infection
Abstract
We examine the intricate clinical management of an 87-year-old Caucasian female with Chronic Obstructive Pulmonary Disease (COPD), who was diagnosed with Mycobacterium abscessus and subsequently co-infected with Klebsiella oxytoca. The resistance of both pathogens to multiple antibiotics complicates treatment significantly. The patient's clinical presentation included chronic symptoms such as dyspnea and productive cough, which were investigated through sputum cultures and bronchoscopy. Despite initial hesitance towards multi-drug therapy, a tailored three-drug regimen eventually led to an improvement in her respiratory symptoms. Highlighting the absence of consensus guidelines for the treatment of Mycobacterium abscessus infections, this case emphasizes the urgent need for definitive treatment protocols. The complexity and rarity of such infections necessitate further research to establish effective management strategies.
Case History
We present an 87-year-old Caucasian female, a former smoker, who had preexisting Chronic Obstructive Pulmonary Disease (COPD) and reported a forced expiratory volume in the first second (FEV1) of 0.84L, and symptoms of dyspnea on exertion, productive cough, clear phlegm, and congestion. She denied any weight loss, fever, chills, or recent exposure to anyone with mycobacterium infections. The patient has had a chronic cough for over two years and has never had a bronchoscopy or sputum culture before for acid-fast bacilli (AFB). Due to high suspicion for atypical mycobacterial infections in a patient with severe COPD and a chronic productive cough, sputum cultures were ordered for AFB and were found positive for mycobacterium abscessus. Patient decided to pursue a single drug regimen against medical advice and was started on azithromycin on an alternate-day basis. Patient continued to have a chronic productive cough. A follow-up computed tomography (CT) chest scan revealed diffuse emphysematous changes, old granulomatous disease, and a right basilar lung mass infiltrate, measuring 2.8 x 1.3 centimeters.
A decision was made to proceed with a diagnostic bronchoscopy. Bronchoscopy results showed no malignancy, however, patient culture results came back positive for rare Klebsiella oxytoca and AFB.
The patient reported a clinical improvement in her breathing post-bronchoscopy. After discussion with the patient, the patient was started on three drug regimens including azithromycin, ethambutol, and rifampin. Rifampin was subsequently discontinued due to side effects.
Discussion
This case report highlights the intricate challenges of managing pulmonary infections caused by Mycobacterium abscessus complex, a rare condition with an occurrence rate of fewer than one case per 100,000 people annually. The complexities are further compounded when co-infections such as Klebsiella oxytoca are present, emphasizing the necessity for tailored therapeutic approaches and multidisciplinary collaboration.
Despite the patient's initial reluctance to initiate a multi-drug regimen, the subsequent positive response to bronchoscopy and symptom improvement following the discontinuation of Rifampin underline the critical role of personalized treatment strategies. This case exemplifies the importance of patient education and active engagement in managing treatment decisions. Moreover, the lack of consensus guidelines by the Infectious Disease Society of America for the treatment of Mycobacterium abscessus infections presents ongoing challenges to clinicians. The reported symptoms of cough and easy fatigability, along with the patient's journey, underscore the need for continued monitoring and follow-up to adjust treatment strategies effectively. The necessity for more research to establish definitive guidelines is evident, as is the importance of a comprehensive approach to manage such complex respiratory infections and balance treatment efficacy with potential side effects.
References
- 1. Griffith, D. E., Aksamit, T. R., & Brown-Elliott, B. A. (2007). An official ATS/IDSA statement: Diagnosis, treatment, and prevention of nontuberculous mycobacterial diseases. American Journal of Respiratory and Critical Care Medicine, 175(4), 367–416. https://doi.org/10.1164/rccm.200604-571st
- 2. Lee, M., Sheng, W., Hung, C., Yu, C., Lee, L., & Hsueh, P. (2015). Mycobacterium abscessus Complex infections in humans. Emerging Infectious Diseases, 21(9). https://doi.org/10.3201/2109.141634
- 3. Prevots, D. R., Shaw, P. A., Strickland, D., Jackson, L. A., Raebel, M. A., Blosky, M. A., De, R. M., Shea, Y. R., Seitz, A. E., Holland, S. M., & Olivier, K. N. (2010). Nontuberculous mycobacterial lung disease prevalence at four integrated health care delivery systems. American Journal of Respiratory and Critical Care Medicine, 182(7), 970–976. https://doi.org/10.1164/rccm.201002-0310oc
-
Bilateral Zephyr Valve Procedures in Severe Emphysema
Abstract
Patients with emphysema often experience persistent dyspnea despite treatment. The FDA-approved Zephyr Valve offers a minimally invasive solution for severe cases, transforming patient outcomes. A 67-year-old Caucasian female, former smoker, underwent successful bilateral Zephyr Valve placement. Initially suffering from severe emphysema and dependent on supplemental oxygen, her first procedure on April 30, 2020, involved placing three valves in the left lower lobe, resulting in significant improvement in dyspnea. Following a relapse, a second procedure on July 22, 2021, placed valves in the right upper lobe, further enhancing her quality of life and reducing symptoms post-rehabilitation. This case underscores that Zephyr Valves can significantly improve life quality and reduce morbidity in patients with severe emphysema. While usually unilateral, bilateral placements have shown promising outcomes, warranting further studies to validate these findings.
Introduction
Patients with severe emphysema often experience persistent shortness of breath and dyspnea despite using COPD medications and supplemental oxygen, due to hyperinflated lungs that cannot release trapped air. The FDA-approved Zephyr® Valve offers a minimally invasive alternative, involving the placement of one-way valves in the airways to help expel trapped air and reduce lung hyperinflation without surgery. While alternative treatments like Lung Volume Reduction Surgery (LVRS) also improve lung function and symptoms, they are more invasive and carry greater risks, making the Zephyr® Valve a preferred option for many. Eligible patients for the Zephyr® Valve must be adults with a confirmed COPD diagnosis, exhibit frequent breathlessness despite medication, and have reduced lung function (FEV1≤50% predicted). Although effective, potential side effects of the procedure include pneumothorax, pneumonia, worsening symptoms, hemoptysis, and chest pain.
Case Presentation
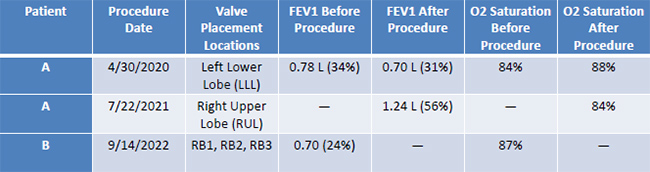
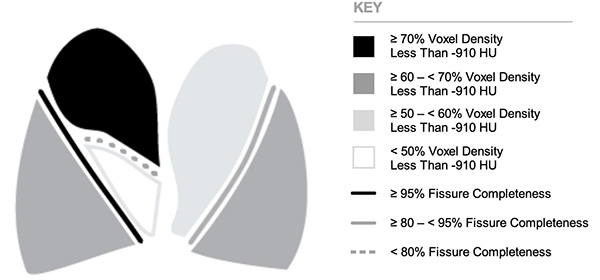
Patient A underwent two Zephyr® Valve procedures on 4/30/2020 and 07/22/2021 for severe emphysema. Initially, two 5 mm and one 4 mm endobronchial valves were placed in the left lower lobe, and later, three valves of varying sizes were placed in the right upper lobe. Pulmonary Function Tests (PFTs) and 6- Minute Walk Tests (6MWTs) were conducted pre- and post-procedures. Initial tests showed an FEV1 of 0.78 L (34% predicted), which improved to 1.24 L (56% predicted) after the second procedure. The patient's oxygen saturation improved slightly, and medication adjustments were made post-procedure due to discomfort with previous treatments.
Patient B received their first Zephyr® Valve on 09/14/2022 and a second on 03/08/2023. Valves were placed in both the right and left bronchi across these procedures. Preprocedure PFTs indicated an FEV1 of 0.70 L (24% predicted), with significant lung hyperinflation noted. A 6MWT pre-procedure showed a decline in O2 saturation to 87, requiring supplemental oxygen. The patient hospitalized for three days post-procedure to monitor for complications. Post-procedure outcome data for Patient B is not yet available.
Discussion
The efficacy of the Zephyr® Valve procedure was analyzed through pre and postprocedure Pulmonary Function Tests (PFTs). For Patient A, initial PFTs indicated a severe obstructive ventilatory defect and reduced diffusing capacity. Post-procedure, these tests revealed moderate to severe defects with variable bronchodilator responses and persistently reduced DLCO. Unfortunately, Patient A's recovery was complicated by COVID-19, which exacerbated her respiratory symptoms and necessitated an increase in oxygen and medication. Patient B experienced dissatisfaction with the procedure's outcomes, coupled with complications like hospital-acquired pneumonia, impacting his respiratory function.
References
- 1. Shafiq, M., Polhemus, E., Perkins, R., Forth, V. E., & Marshall, M. B. (2022). Bilateral bronchoscopic lung volume reduction after surgical fissure completion. Chest, 162(2), e73–e75. https://doi.org/10.1016/j.chest.2022.02.005
- 2. Criner, G. J., Sue, R., & Wright, S. E. (2018). A multicenter randomized controlled trial of Zephyr endobronchial valve treatment in heterogeneous emphysema (LIBERATE). American Journal of Respiratory and Critical Care Medicine, 198(9), 1151–1164. https://doi.org/10.1164/rccm.201803-0590oc
- 3. Zephyr Valve treatment for COPD and emphysema | University of Michigan Health. (n.d.). https://www.uofmhealth.org/conditions-treatments/pulmonary/zephyr-valve-treatment-copdemphysema
-
A Case of Eosinophilic Pneumonia
Introduction
Eosinophilicpneumonia (EP) is a rare respiratory disorder characterized histologically by eosinophilic infiltration and interstitial inflammation.
The disease process of this conditionis thought to involve an aberrant immune response in which eosinophils play a central role. Eosinophils are typically recruited to the lungs by eotaxin, a specific chemokine, and other cytokines, leading to inflammation and, eventually, lung tissue damage.
EP can manifest in one of two forms an acute variant whichoften presents with rapid onset of severe respiratory symptoms, including dyspnea and hypoxemic respiratory failure and a chronic variant which presents withchronic cough, weight loss, night sweats, and gradually worsening dyspnea.Both forms respond well to corticosteroids, underscoring the inflammatory nature of the diseases.
Case Presentation
- 1. We report the case of a 66-year oldCaucasianmale with ahistory of diabetes mellitus and no past medical history ofsmoking whose symptoms include a productive cough withclear phlegm, SOB, and chest pain.
- 2. Chest CT revealed mildly prominent bilateral hilar lymph nodes, nodularity involving the right lobe posteriorly, and emphysematous changes seen at the periphery of the upper lobes. PET scan revealed mild ethmoid sinus mucosal thickening as well as hypermetabolic mediastinal and hilar lymph nodes.
- 3. Findings from these scans were corroborated into a mediastinal lymphadenopathy diagnosis for which a mediastinoscopy was ordered to rule out any malignancy or mycobacterial/fungal etiologies. Results from the mediastinoscopy returned as negative.
- 4. Patient’s bronchitis persisted despite antibiotics, thus a sputum stain for AFB and sputum fungal culture were ordered but returned negative. Follow up chest CT showed an increase in mediastinal lymph node enlargement, pleural effusion, para-septal emphysema, new areas of ground glass opacities with a central component, and mild bronchial wall thickening in the mid and lower lung zones.These findings are consistent with possible AEP.
- 5. Following the emergence of vasculitis manifesting as a petechial rash on his lower extremities, upper extremities, and back aCT guided and endobronchial biopsy were performed. Results from the biopsy showed focal squamous metaplasia of the mucosal lining and lymphocytes and eosinophils in the submucosa as well as a BAL cell count of 70% EOS which confirmed the diagnosis of AEP.
- 6. The patient was started on a regimen of high-dose prednisone and Bactrim for prophylaxis against potential secondary infections, with follow-up planned to assess response to therapy and adjust treatment as necessary.
Discussion
This case exemplifies the multifaceted and often protracted diagnostic process for eosinophilic pneumonia (EP), a rare but serious condition characterized by eosinophilic infiltration of the lung parenchyma. The patient's initial symptoms and radiographic findings suggested more common respiratory conditions, leading to a series of evaluations and treatments before arriving at the diagnosis of acute eosinophilic pneumonia (AEP).
Diagnostic Complexity and Role of Imaging
The diagnostic journey highlights the central role of advanced imaging and cytological analyses in diagnosing EP. Persistent mediastinal lymphadenopathy, initially attributed to recurrent bronchitis and other benign causes, was later linked to eosinophilic infiltration through more targeted investigations. Advanced imaging techniques such as high-resolution computed tomography (HRCT) are critical in distinguishing EP, showing peripheral or diffuse ground-glass opacities typically absent in routine evaluations (Johkoh et al., 2000).
Eosinophilic Pneumonia in Atypical Demographics
This patient's age and absence of typical risk factors, such as smoking or occupational exposures, underscore the need to consider EP across a broad demographic spectrum. Literature suggests that while EP commonly affects younger males, cases in older adults should not be overlooked. As discussed by Cottin et al. (2023), eosinophilic lung diseases do not strictly adhere to a specific demographic and can vary widely in presentation and severity[4].
Treatment Efficacy and Management Challenges
The administration of corticosteroids resulted in marked clinical improvement, aligning with guidelines that recommend steroids as the frontline treatment for EP (Naughton et al., 1993) [4]. . However, the necessity to reintroduce medication highlights the episodic nature of EP, where flare-ups are common and may require long-term management strategies.
Implications for Long-term Monitoring
The recurrence of symptoms upon discontinuation of therapy underscores the importance of careful long-term monitoring and the potential need for maintenance therapy. Research suggests that a graduated tapering of corticosteroids can effectively prevent relapses in EP, necessitating a careful balancing of treatment duration and side effects (Badesch et al., 1989).
Chronic vs. Acute Eosinophilic Pneumonia
AEP presents abruptly and is often severe, with patients experiencing acute respiratory failure. The symptoms of AEP include rapid onset of febrile illness, hypoxemia, and diffuse pulmonary infiltrates on imaging (De Giacomi et al., 2018)[2]. Radiographically, CEP is known for its peripheral opacities, often described as a "photographicnegative of pulmonary edema" (Marchand et al., 1998)[1].Treatment involves corticosteroids for both forms; however, the duration and tapering schedule may differ significantly between CEP and AEP, with CEP often requiring longer-term management to prevent relapse.Bronchoalveolar lavage (BAL) is critical in diagnosing both forms but is particularly indicative in AEP, where an eosinophilic count of over 25% can often be observed, compared to a more variable count in CEP.
Research Gaps and Future Directions
The idiopathic nature of this case points to significant gaps in our understanding of EP's etiology. Ongoing research into the autoimmune or allergic triggers could provide deeper insights into more effective, targeted treatments beyond corticosteroids. Additionally, this case's brief consideration of eosinophilic granulomatosis with polyangiitis (EGPA) as a differential diagnosis illustrates the overlap in clinical features and the importance of distinguishing between these conditions for optimal management outcomes.
 Frontal View of AEP Patient CXR
Frontal View of AEP Patient CXR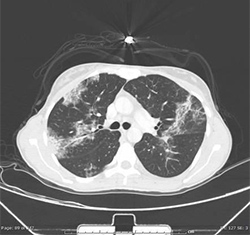 Axial Lung Window of AEP Patient
Axial Lung Window of AEP Patient Frontal View of Normal CXR
Frontal View of Normal CXR
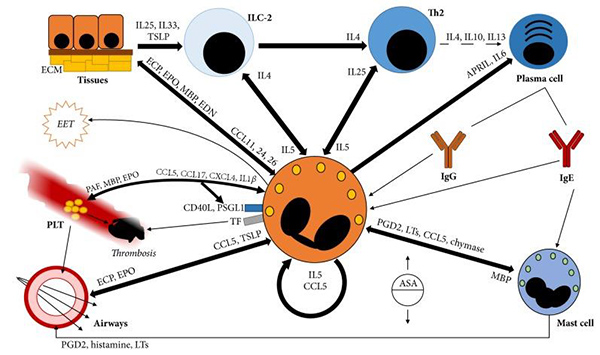
Eosinophils are central to inflammatory responses and interact with various cells, enhancing immune reactions through cytokine signaling with ILC-2, Th2 cells, and mast cells. These interactions are crucial in respiratory conditions, including eosinophilic pneumonia, where eosinophils contribute to tissue inflammation and remodeling. They activate and sustain ILC-2 and Th2 cells, which in turn promote eosinophil survival and activity via IL5 and IL25. Additionally, eosinophils interact with mast cells, triggering the release of inflammatory mediators like leukotrienes, which are particularly significant in eosinophilic respiratory disorders. Through these mechanisms, eosinophils play a pivotal role in the pathogenesis of eosinophilic pneumonia by disrupting tissue integrity and exacerbating inflammation.
References
- 1. Marchand, E., Reynaud-Gaubert, M., Lauque, D., Durieu, J., Tonnel, A.-B., & Cordier, J.-F. (1998). Idiopathic chronic eosinophilic pneumonia: A clinical and follow-up study of 62 cases. Medicine, 77(5), 299–312. https://doi.org/10.1097/00005792-199809000-00001
- 2. De Giacomi, F., Vassallo, R., Yi, E.S., Ryu, J.H. (2018). Acute eosinophilic pneumonia. Causes, diagnosis, and management. American Journal of Respiratory and Critical Care Medicine, 197(6), 728-736.
- 3. Johkoh, T., et al. (2000). Eosinophilic lung diseases: Diagnostic accuracy of thin-section CT in 111 patients. Radiology, 216(3), 773-780.
- 4. Cottin V. (2023). Eosinophilic Lung Diseases.Immunology and allergy clinics of North America,43(2), 289–322. https://doi.org/10.1016/j.iac.2023.01.002
- 5. Naughton, M., Fahy, J., FitzGerald, M. X. (1993). Corticosteroids and treatment of eosinophilic pneumonia. Chest, 103(1), 166-169.
- 6. Badesch, D. B., et al. (1989). Pulmonary eosinophilia evaluated by bronchoalveolar lavage. American Review of Respiratory Disease, 139(2), 494-497.
- 7. Sadowski, L., et al. (2021). Eosinophilic pneumonia: Mechanisms, clinical presentations and management. Annals of Allergy, Asthma & Immunology, 126(5), 477-484.
- 8. Gaillard F, Normal chest x-ray. Case study, Radiopaedia.org https://doi.org/10.53347/rID-8304
- 9. Ramirez, G. A., Yacoub, M. R., Ripa, M., Mannina, D., Cariddi, A., Saporiti, N., Ciceri, F., Castagna, A., Colombo, G., & Dagna, L. (2018). Eosinophils from Physiology to Disease: A Comprehensive Review.BioMed research international,2018, 9095275. https://doi.org/10.1155/2018/9095275

